26th November 2017
State of Health in the EU: The Czech Republic performs well in terms of allocating resources efficiently to various care sectors. But there is real scope for technical efficiency improvements
Within its State of Health in the EU project, the European Commission tracks national specificities and progress made in the area of health and health care system in each member state. Country profiles.
Key findings for the Czech Republic
- The Czech health system has made major advances in population health. Despite historically high mortality from certain diseases, a majority of health-related indicators are closing the gap with EU averages. Moreover, recent developments in survival rates from cancer and 30- day mortality from cardiovascular diseases are likely to continue this trend. Preventable mortality indicators reveal a more mixed picture. The rising prevalence of diabetes is worrisome, as are the high mortality rates from traffic accidents and liver diseases.
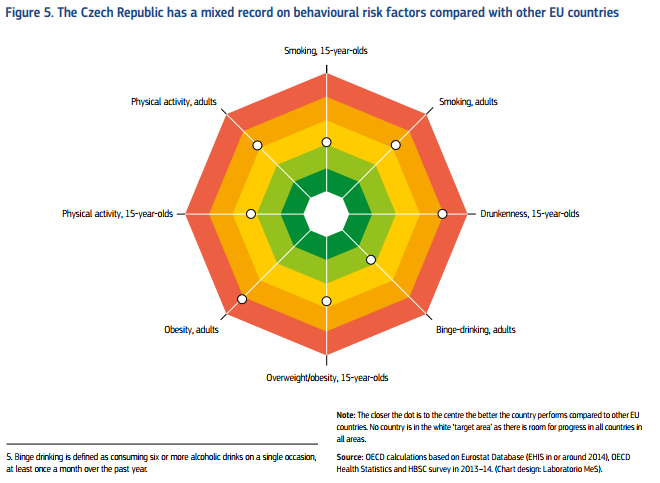
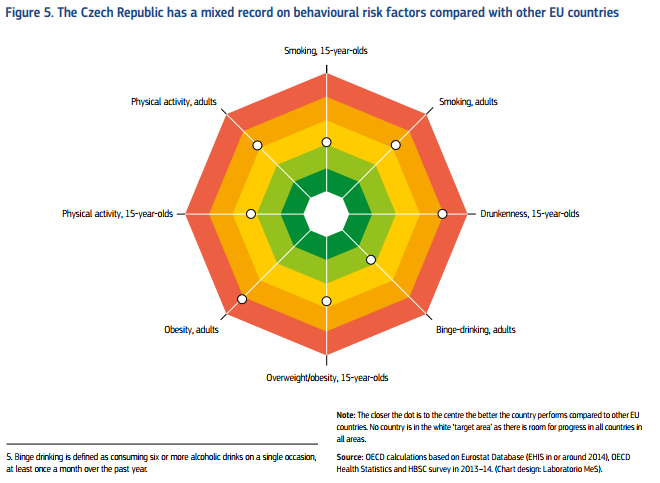
- The public health system has expanded its role over the last five years and now holds responsibility for non-communicable diseases. However, work to tackle the high prevalence of risk factors is still in its infancy. Tobacco control legislation has been strengthened, but programmes targeting alcohol consumption and rising obesity have yet to prove effective.
- The Czech Republic maintains a high level of financial protection with universal coverage, a very generous benefit package and low out-of-pocket spending. There is legislation to protect vulnerable groups, including an annual ceiling on co-payments for low income households. As a result, levels of unmet needs for financial reasons are among the lowest in the EU.

Source: European Commission, State of Health in the EU 2017, country reports
- There are, however, questions about adequacy of the current health financing system, particularly given the narrow revenue base, its vulnerability to shocks and the likely impact of population ageing on the dependency ratio and on levels of contributions to the system.
- There are also concerns about the ageing of the health workforce, the uneven distribution of doctors, migration abroad, GP vacancies in rural areas and travel distances. Numbers of primary care physicians are a particular worry, because it is not perceived as an attractive specialisation. All these factors raise questions about the availability of services in the long term and potential barriers to access. A comprehensive response would focus on training, retention policies and incentive schemes to avoid shortages in the medium and long term.
- The long-term care infrastructure can be characterised by regional disparities and a need for modernisation. There is a need to diversify long-term care delivery to treat people in their communities and at home, as well as to strengthen coordination and integration in health care and social care and across different providers. Currently, there is only a low degree of coordination between providers, which is further hindered by lacking eHealth solutions. Recent legislation to tackle this may be a step in the right direction.
- The Czech Republic performs well in terms of allocating resources efficiently to various care sectors. But there is real scope for technical efficiency improvements. Primary care could be strengthened so that it provides care in the most cost-effective setting and becomes an effective gatekeeper. Hospitals could reduce bed numbers and improve on indicators like average length of stay or occupancy rates. A Health Technology Assessment system could be developed to improve coverage decisions.